American Oversight
An informed public,
a strengthened democracy.
Timeline: Early Communications and Confusion Around Coronavirus

In the early months of the coronavirus pandemic, U.S. officials scrambled to respond to the growing threat, encountering problems with testing, shortages of personal protective equipment, and a Trump administration frequently focused on politics over public health. Records obtained by American Oversight shed light on these issues as well as early assessments about the virus — including the prevalence of asymptomatic transmission and the effectiveness of wearing masks — and poor coordination between the administration and state officials. Below is a timeline of communications and documents from January through April of 2020, uncovered through Freedom of Information Act requests and litigation, that provide insight into these challenges.
Jan. 6, 2020: Robert Redfield sent a letter to Dr. George Gao, head of China’s Center for Disease Control and Prevention, offering assistance in light of reports about “the cluster of pneumonia of unknown etiology” at “a local seafood market” in Wuhan. “I would like to offer CDC technical experts in laboratory and epidemiology of respiratory and infectious diseases to assist you and China CDC,” Redfield said.
Jan. 30, 2020: Assistant Secretary of Defense Ken Rapuano emailed Robert Kadlec, the assistant secretary for preparedness and response at HHS, asking for Kadlec’s takeaways from a recent meeting, because Rapuano had been “receiving multiple feeds and they’re not all consistent.” Kadlec responded, “[Undersecretary of Defense James] Anderson represented DOD […] and I am not sure he may have heard or gotten all that transpired in the room or heard what was tasked because it was fairly vague. The dilemma is State is looking to move 700+ all at the same time. That was a shocker and one that we had not anticipated.” Kadlec was potentially referring to the evacuation of Americans from Wuhan and nearby areas.
Feb. 1, 2020: An early press guidance from the National Security Council emphasized containment in China through quarantine and travel restrictions. The guidance stated that “the risk of infection for Americans remains low” and that “It is likely that we will continue to see more cases in the United States in the coming days and weeks, including some limited person-to-person transmission.”
Feb. 20, 2020: CDC official Darin Carroll asked colleagues Chris Elkins and Stephen Lindstrom, the head of the CDC Respiratory Viruses Diagnostic Laboratory, to run samples that had been split between two labs, from two patients. Lindstrom replied in confusion, and later said, “We need to discuss and resolve a number of issues.”
Feb. 23, 2020: Dr. Eva Lee, a public health and disease-modeling expert, sent an email detailing information about how seemingly healthy individuals, despite testing negative, can spread the virus during its incubation period. Robert Kadlec replied, “Eva Is this true?! If so we have a huge [hole in] our screening and quarantine effort.”
March 5, 2020: A senior adviser to Centers for Medicare and Medicaid Services Administrator Seema Verma emailed CDC officials to schedule a call about nursing homes. She said, “It has been difficult to get [Assistant Secretary Kadlec’s office] on board with the nursing home call today so we are going to aim for first thing tomorrow morning. I know Dr. Redfield is getting in super early to Atlanta, but hoping we can find a time to have the first call tomorrow since it is most important that Adm Verma and Dr. Redfield be on the line.” This was forwarded to CDC Chief of Staff Robert McGowan, who said, “He [Redford] can’t do anything tomorrow before 12:30.” The documents do not indicate whether or when the call took place.
March 8, 2020: On a phone call, representatives from Kaiser Permanente and HCA Healthcare requested “immediate consideration for modification of current [CDC and CMS] guidance,” according to an email sent to testing coordinator Brett Giroir and other health officials. Among their concerns were “aerosol level personal protective equipment versus respiratory droplet,” which suggests that health officials were aware at this time about the possible spread of the coronavirus through tiny aerosols as opposed to only larger droplets. Another recommendation suggested that Covid-positive but asymptomatic health care workers be allowed to work if wearing proper PPE.
For more than a year, health experts had warned that the CDC’s focus on “close contact” as the primary way the virus spread ignored the prevalence of aerosol transmission. In September and October 2020, the CDC published, removed, and republished guidance on its website stating that “some” Covid-19 infections were spread through aerosols. In May 2021, updated guidance again acknowledged aerosol transmission and stated that it was not uncommon for the virus to be transmitted beyond 6 feet. In March 2022, the White House stated that the most common way the virus is spread is “through tiny airborne particles of the virus hanging in indoor air for minutes or hours after an infected person has been there,” a statement with important implications for indoor air ventilation in buildings across the country.
March 11, 2020: Former DHS Secretary Kirstjen Nielsen pitched ANDE, a corporation specializing in rapid DNA technology with long-standing government ties, to help with Covid-19 testing. She wrote to HHS Secretary Alex Azar, “I know about them b/c I had hoped we could deploy rapid DNA technology on our southern border for a variety of reasons.”
March 14, 2020: A White House staff secretary asked for feedback on an attached draft “mass-mailing postcard from the President with information on how to protect yourself from COVID-19 and what to do if you have symptoms.” The email requested feedback by 7 p.m. that evening and was sent to Anthony Fauci, Deborah Birx, and several top administration and White House officials. The draft postcard included guidance to “wear a mask if you have any respiratory symptoms to protect your household.” A follow-up email from the staff secretary detailed feedback from staff, including a comment about whether the mask guidance would be confusing given the White House’s messaging. “We (and [White House Coronavirus Task Force] members) have been saying only medical professionals should wear masks, so just want to be sure we’re being consistent,” the comment said. The final version of the postcard did not include the guidance on mask-wearing and was delivered to households throughout the country beginning March 21.
March 15–19, 2020: In a March 15 text message conversation with Mark Meadows, who had not yet officially resigned from Congress to become White House chief of staff, HHS Secretary Alex Azar apologized for apparent issues with an FDA contact number. “The entire point of having the FDA commissioner on the phone was to get their issue solved not to give them a nonworking phone number,” Azar said. “I instructed him to speak to the lab and fix their issue directly and then to call the number and find out why it isn’t working.”
On March 19, Azar messaged Meadows regarding an unidentified potential supplier of personal protective equipment. Azar wrote, “So on N95 guy, not a Nigerian prince but just about. He’s offering 2/3 of the national utilization in a year. We asked for lot numbers to confirm with [mask supplier] 3M. He offered to DHS, DOD, and NSC and all took a pass. Will let you know but he looks like a potential charlatan.”
Azar then wrote, “As for DOD, we have no idea what this issue is as we haven’t asked for DOD to help with testing and our leadership wasn’t aware of any kind of offer from DOD.” Azar added that the Defense Department’s Ken Rapuano had told him the department had the capability to run 60 tests per day. “We certainly appreciate the offer but with commercial labs doing 20,000 yesterday not sure this is a material offer. … DOD [chief of staff] has no idea what any of this is about but we found [Secretary Mark] Esper’s statement at press conference offering civilian use. So we will send a request tonight to them. They can sort out if they can live up to it or not.”
March 23–24, 2020: Dr. Yuen Kwok-yung, a microbiologist based in Hong Kong, copied Deputy National Security Adviser Matthew Pottinger on an email to a Wall Street Journal reporter who had asked about whether mask-wearing helped contain the coronavirus’s spread. Yuen said that mask-wearing would “markedly reduce the community transmission” and explained “why most medical colleagues in [Hong Kong] advocate universal masking once leaving their home.”
March 31, 2020: A CDC official circulated notes from a phone call with Sen. Pat Toomey held two days before. During the call, Toomey and CDC officials discussed mask-wearing, including the effectiveness of different types of masks and “[p]ossible confusion/misinterpretation/unintended consequences re: CDC guidance on use of masks.” Toomey asked the CDC to clarify guidance on mask-wearing.
April 1, 2020: Anne Schuchat, the CDC’s principal deputy director, emailed CDC officials with notes from a press briefing with Trump. She noted that Trump said people who want to wear a mask “could wear a scarf if they wanted to.” Schuchat added that during the briefing, Birx had said that “the broader question” of whether everyone should wear a mask was still being discussed by the White House task force.
April 2, 2020: Anne Schuchat said, “The STAG-IH [the World Health Organization’s Strategic and Technical Advisory Group for Infectious Hazards] is discussing the community mask issue and most of us have moved our opinions based on the Asian experience and the relevance of presymptomatic transmission. We also have been discussing the homemade option so it shouldn’t be so inaccessible for low resource places. … But we are reviewing evidence on Friday’s morning call.”
April 7, 2020: In a text message to FDA Commissioner Stephen Hahn, FDA Senior Adviser Colin Rom wrote, “Tests are going to [National Cancer Institute] not CDC. CDC was involved in all the communications that alerted folks to [the] fact [that] tests were going to NCI. Looks like might just be miscommunication within CDC.” Hahn asked Rom to have FDA Deputy Commissioner Anand Shah alert Schuchat so she could coordinate with Redfield.
April 13, 2020: A representative from Palmetto Citizens Federal Credit Union expressed frustration about not being able to submit Paycheck Protection Program loan applications through an online portal, and wrote that local Small Business Administration representatives were unable to assist. “We have lost faith in the entire program/process at this point.” The email was forwarded to SBA officials by someone who appears to be a consultant.
April 2020: Records reveal that ICE prioritized deportations over migrant safety by failing to test all people for Covid-19 before deportation flights. On April 17, the government of Jamaica sent a letter to DHS asking that all deportees take rapid tests prior to flying, writing that ICE’s planned temperature checks were not sufficient. According to an April 30 flight updates email from Marlen Pineiro, assistant director of ICE Enforcement and Removal Operations (ERO), the Guatemalan government requested that people deported from the U.S. be tested and that their negative results be sent for approval prior to the flight. “This is very logistically difficult and will add an additional detention day,” Pineiro wrote.
April 28, 2020: A CMS official sent an email with the subject line “nursing home study & sports,” saying that officials “met with the professional sports leagues today. Is the CDC planning on putting out guidelines for little leagues, etc community sports?” Anne Schuchat replied, “CDC subject matter experts did some individual consultations with Major League Baseball, National Football League, and National Basketball Association as well as with Little League. We hadn’t developed guidance for general release for professional sports. … If you have specific suggestions of what you think would be useful in terms of sports our staff are happy to follow up.”
 American Oversight obtained numerous records of communications of officials at the Department of Veterans Affairs about the agency’s response to the pandemic. One set of email messages revealed that senior federal health officials were increasingly alarmed about the rapidly spreading virus in late February and early March, even as President Trump and other top officials were publicly downplaying the threat of the virus.
American Oversight obtained numerous records of communications of officials at the Department of Veterans Affairs about the agency’s response to the pandemic. One set of email messages revealed that senior federal health officials were increasingly alarmed about the rapidly spreading virus in late February and early March, even as President Trump and other top officials were publicly downplaying the threat of the virus.
In February 2020, the U.S. worked to bring Americans who were abroad back to the country. Paul Kim, the executive director of the Veterans Health Administration’s Office of Emergency Management, sent regular emails detailing VA emergency personnel’s involvement in this repatriation. On Feb. 16, Kim sent updates about the repatriation of passengers from the Diamond Princess cruise ship. He stated that two veterans had been identified on the ship and that many of the evacuees “expressed anger at the US Govt. due to the requirement to be quarantined for an additional 14 days upon their arrival on US soil.”
Feb. 28, 2020: Carter Mecher, a VA senior medical adviser, wrote that “we are flying blind” with regard to the lack of Covid-19 mitigation measures in place in the United States.
March 9, 2020: Mecher warned that “time is being frittered away. It has been 9 days since Seattle announced the first death. They really haven’t put measures in place that will tamp down transmission. They have lost valuable time that cannot be made up. Time = transmission = more ill = more hospitalized = more dead = overwhelmed healthcare = failure. Can’t be any more direct than that.”
March 13, 2020: The National Nurses United union complained about the VA’s pandemic response, saying that the “VA is either unwilling and/or unprepared to answer basic questions that will ensure the safety of RNs and the patients who they are taking care of.” The group also said the VA was not providing nurses with sufficient personal protective equipment.
April 27, 2020: Notes and talking points for a call between VA Secretary Robert Wilkie and the CEO of 3M, a supplier of N95 masks, said that the VA’s demand for 3M masks had increased more than 6,000 percent and that the agency was struggling to make up the shortfall. One of the talking points was “We understand that FEMA/White House has levied three Defense Production Act rated contract agreements for 3M, shifting all their production to support the National Emergency, which has greatly impacted the Department’s existing supply chain agreements.”

Jan. 31, 2020: After the CDC updated its criteria for evaluating patients under investigation to include anyone who had traveled to mainland China and who was experiencing fever and symptoms requiring hospitalization, Dr. Ryan Westergaard, the Wisconsin Department of Health Services’ chief medical officer, emailed colleagues: “This does not make sense strictly from a public health perspective, since many confirmed cases have not had severe symptoms requiring hospitalization,” he wrote. “I hope as the lab capacity increases they will revisit this.”
Feb. 1, 2020: Jerrod Davis, Washington state’s assistant health secretary, wrote, “Yesterday’s [White House] briefing was a bombshell. Our team is rolling up their sleeves to pivot accordingly.” At the briefing, Trump had declared coronavirus a public health emergency and had announced travel restrictions, including mandatory quarantine for U.S. citizens returning from the Hubei province and a ban on non-citizens traveling from China.
Feb. 6, 2020: CDC officials requested that Florida officials start using the CDC’s system for data collection, called DCIPHER. The CDC followed up with Florida repeatedly, asking state officials on Feb. 12 and Feb. 15 to designate staff to manage the Covid-19 data. Florida officials replied, “Per previous conversations, we will not be using DCIPHER.”
Feb. 21, 2020: A CDC epidemiologist asked Scott Lindquist, a Washington state health official, if it would be feasible to collect serum from close contacts of those infected, to determine whether there were an immune response to the coronavirus. Lindquist agreed that such a strategy would be good, but added that “the logistics of contacting, consenting and arranging the blood draws are beyond local staffing.”
March 1, 2020: An official from King County, Wash., emailed a CDC official asking for clarification on guidance on whether asymptomatic people who had been in close contact with cases should quarantine. “The CDC recommendation is to be quarantined,” the CDC official responded. “However, if the county wants to loosen that policy given the shortage of [health care personnel], perhaps having these asymptomatic contacts wear masks is acceptable. That would be your call.”
March 2, 2020: Daniel Jernigan, the director of the CDC’s Influenza Division, told colleagues that Texas officials were frustrated with the unreliability of the CDC’s test.
March 11, 2020: Florida epidemiologist Ann Schmitz responded to a query from a health official regarding guidance about testing asymptomatic individuals, as requested by physicians and hospital laboratories. Schmitz said that the Florida Department of Health was “not recommending testing of asymptomatic persons, though as you are aware a handful of exceptions were made for the cruise industry.” At the time of Schmitz’s communication, it was public knowledge that there was already community spread of the coronavirus in Florida.
March 15, 2020: Anne Caprara, the chief of staff for Illinois Gov. J.B. Pritzker, wrote: “On the testing issue – my boss has been calling White House officials, including the Vice President, about this for two weeks. To be quite honest, we’ve all given up getting a straight answer from you guys.”
March 20, 2020: In a Slack conversation, state health officials discussed possible explanations for a drop in emergency hospital visits. They suggested that the decline might be due to public health messaging encouraging social distancing, more telehealth visits, or hospitals redirecting respiratory patients to other health centers.
March 24, 2020: Florida health official Sharon Denton-Gow emailed Florida officials about testing shortages. In a separate email to several officials, she wrote: “Please also understand that there are nearly 50K first responders in the Miami, Broward, Palm Beach foot print and we are limited to 250 tests per day.”
March 29, 2020: An official in HHS’s Office of the Assistant Secretary for Preparedness and Response circulated an email that included recommendations for a total of 1,150 ventilators to be provided to Connecticut; Chicago, Ill.; New Jersey; and Michigan. The email noted that “there would be 9,354 vents remaining” in the Strategic National Stockpile if these numbers were to be approved and recommended 300 ventilators for Connecticut. In a reply, Brett Giroir pointed out that the state has 584 adult ventilators available, writing, “I am not sure why we send them an additional 300. You can pick a number much smaller — 100?”
An updated email sent later that day recommended 50 ventilators for Connecticut. At a White House press briefing on April 2, Jared Kushner came under fire for saying that the Strategic National Stockpile was “not supposed to be states’ stockpiles that they then use.”
April 14, 2020: State health officials discussed over Slack whether to make Covid-related syndromic data publicly available. “I’d strongly encourage transparency,” wrote an official from New York.
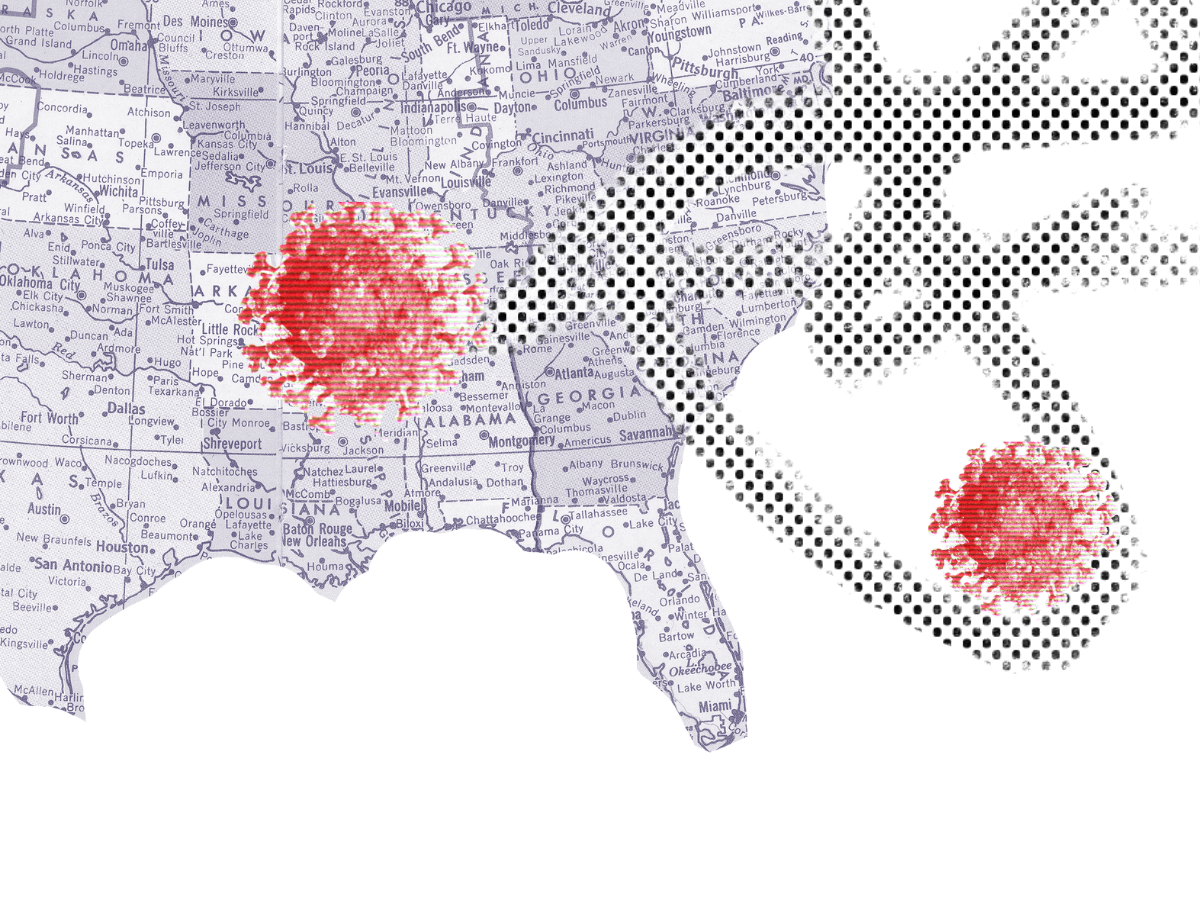
July 6, 2020: Audrey Arona, the Georgia Department of Health’s director for Gwinnett, Newton, and Rockville counties, wrote to Surgeon General Jerome Adams about the state’s difficulty managing its high number of Covid-19 cases. Arona wrote that local officials were “unable to investigate all cases fully and despite educating cases and contacts about isolation and quarantine, as appropriate, there is no capacity to ensure that these disease control measures are maintained.” She also noted the lack of experience of hired contact tracers and said that epidemiologists were spending significant amounts of time “trying to manage and lead hordes of inexperienced staff conducting the investigations and contact tracing.”
Arona asked the Trump administration to implement a national educational campaign about exposure, testing, and isolation periods. “All contacts are recommended to quarantine for 14 days after their last exposure to the case … and schedule testing around day 10 of their quarantine period.” Arona expressed concern about individuals who were getting tested immediately after exposure and forgoing quarantine requirements when they test negative. “Educating them to test later in their quarantine period will give a more accurate assessment of their true disease status and reduce unnecessary testing.” On July 7, Adams forwarded Arona’s email to Birx, Redfield, Fauci, and others.